In this episode, I’ll discuss alternative anticoagulation strategies for continuous renal replacement therapy during the calcium shortage.
According to the ASHP current drug shortages list, both calcium chloride and calcium gluconate are in short supply due to manufacturing delays.
The “local anticoagulation” method of using citrate during continuous renal replacement therapy requires large amounts of IV calcium. In a shortage situation, alternative means of anticoagulation may be required.
Citrate anticoagulation
Here is how local anticoagulation with citrate works:
Citrate is infused into the extracorporeal blood circuit during continuous renal replacement therapy. The citrate binds ionized calcium, which inhibits coagulation of the blood while it is in the circuit. While not commonly referred to as such, calcium is also known as “clotting factor IV.” Calcium is a necessary cofactor for coagulation; When levels of ionized calcium are severely decreased, blood becomes incoagulable.
Calcium is then infused into the patient to keep the level of ionized calcium sufficient for normal coagulation and hemostasis to occur in vivo. This method is referred to as local or regional citrate anticoagulation (RCA) because blood is only anticoagulated while it is in the circuit. RCA does a better job keeping the CRRT circuit patent while having less risk of bleeding compared with other anticoagulation strategies such as heparin infusion.
Alternative means of anticoagulation
If calcium is unavailable, citrate based anticoagulation cannot be used. Alternative means of anticoagulation include systemic unfractionated heparin or argatroban infusions.
The risk of bleeding must be considered when deciding to use systemic anticoagulation during CRRT. The use of full intensity anticoagulation is unnecessary. The minimum amount of anticoagulation required to achieve a reasonable filter life should be used. A filter life of 24 hours is generally considered reasonable. Several factors must be taken into consideration to minimize bleeding risk:
Recent surgery
Recent history of bleeding
Platelet count
INR
aPTT
Heparin
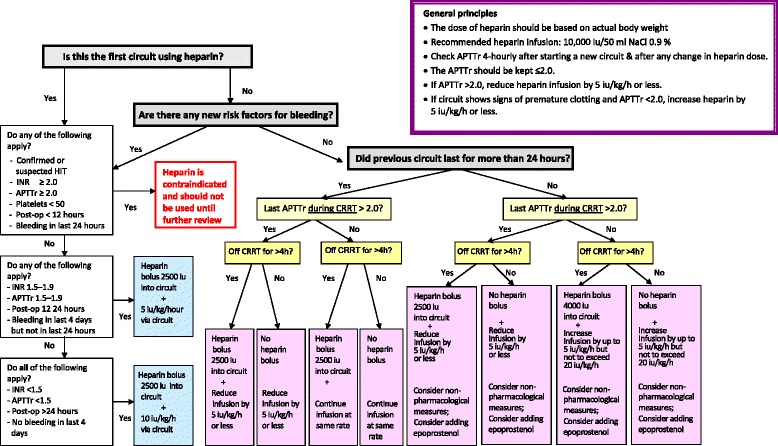
A heparin based protocol for anticoagulation during CRRT has been published in the open access journal Critical Care.
A heparin bolus of 2500 units and infusion of 10 units/kg/hr into the circuit are used for patients who have a low bleeding risk and meet the following criteria:
INR <1.5
aPTT <1.5 times normal
Platelets > 50,000
No surgery in past 24 hours
No bleeding in past 96 hours
A heparin bolus of 2500 units and infusion of 5 units/kg/hr into the circuit are used for patients who have a moderate bleeding risk and meet the following criteria:
INR 1.5 to 1.9
aPTT 1.5 to 1.9 times normal
Platelets > 50,000
No surgery in past 12 hours
No bleeding in past 24 hours
Heparin is not indicated for use during CRRT if the patient has a high risk of bleeding or meet any of the following criteria:
INR 2 or more
aPTT 2 or more times normal
Platelets < 50,000
Surgery in past 12 hours
Bleeding in past 24 hours
Confirmed or suspected HIT
Suggested heparin protocol
Argatroban
In patients with HIT who require anticoagulation to achieve a reasonable CRRT filter life, argatroban may be considered. To my knowledge argatroban has only been studied in 30 patients for this purpose. A bolus of 100 mcg/kg is given and the starting infusion dose is based on the degree of critical illness. A formula proposed to determine the infusion rate in mcg/kg/min is as follows:
2.15- (0.06 x APACHE II score)
or
2.06- (0.03 x SAPS II score)
If the patient has severe liver disease, I would not start the argatroban infusion higher than 0.5 mcg/kg/min. Remember that the INR is falsely elevated when using argatroban, and therefore cannot be used to evaluate bleeding risk.
Bivalrudin
Bivalrudin has also been used for anticoagulation during CRRT although published evidence is limited to 5 patients. The dose used in this study was 2mg/hr.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
Leave a Reply