In this episode I’ll discuss my ICU workflow as a critical care pharmacist. I’ll also share how I orient PGY-1 pharmacy residents to my critical care pharmacy rotation.
Workflow
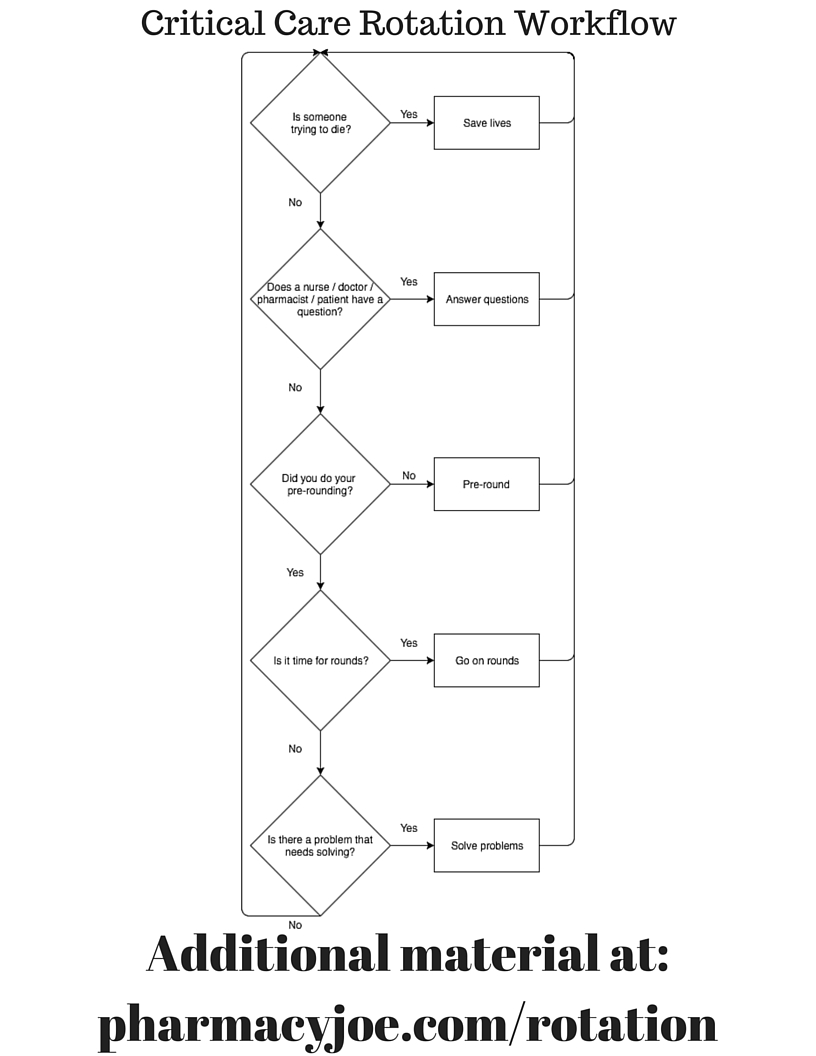
There is a basic workflow to the critical care pharmacy rotation, and I’ve captured it in a diagram using the tool draw.io:
You can download a PDF of this Critical Care Pharmacist Workflow diagram in my free download area.
Other than assigned projects, the tasks performed by students and residents on rotation come down to:
1. Responding to medical emergencies
2. Answering questions and solving pharmacotherapy related problems
3. Getting ready for and participating in ICU rounds
PGY-1 Rotation Orientation
One of the great things about having this podcast is that I can have my residents and students listen to selected episodes before starting rotation with me. Face-to-face orientation time gets spent on in-depth discussions rather than just a review of the basics. This is ultimately better for patients because I spend less time getting the resident or student up to speed before we can get to work solving patient care problems.
In addition to reviewing the rotation workflow with the resident I have them listen to 4 previous podcast episodes. These episodes are summarized in this post. I have also compiled them in one place at pharmacyjoe.com/rotation. Feel free to use that page in your orientation procedure as well.
The 4 episodes cover:
1. Verbal communication
2. Patient assessment
3. Getting ready for ICU rounds
4. Participating in ICU rounds
This is the orientation I use for PGY-1 residents, but it can also be used for APPE pharmacy students. My rotation is much more intense and in-depth for a pharmacy resident than a student, but the general orientation points are the same.
Verbal communication with providers
I covered verbal communication with providers in episode 9 which is titled: How to talk like a physician and get a physician to listen like a pharmacist.
I have residents use a tool called ISBAR to collect their thoughts and learn how to talk like a physician and get the physician to listen like a pharmacist.
Introduction
Situation
Background
Assessment
Recommendation
Until it becomes 2nd nature, the resident should literally sketch out the conversation before it happens using the ISBAR tool on paper.
For more detail on verbal communication I have the resident listen to episode 9.
Making patient focused risk:benefit assessments
To help the resident begin to learn to make patient focused risk:benefit assessments, I give them a basic explanation of why a patient might be in the ICU. Focusing on what exactly is requiring the patient to be in the ICU helps me identify and prioritize patient problems.
From my point of view in an open medical/surgical ICU there are 3 reasons for ICU admission:
1. One or more of a patient’s vital organ systems has failed and we need to support them. This could be respiratory failure from pneumonia, or post-ROSC care of a cardiac arrest patient, or hypotension requiring vasopressors from sepsis.
2. Something happened to the patient that places them at high risk of a vital organ system failing, and we want to immediately recognize and support it if/when that happens. This could be watching a patient for 24 hours after alteplase for acute ischemic stroke, or a patient who just had a high risk surgical procedure, or a patient with delirium tremens requiring high doses of benzodiazepines.
3. Politics. The patient knows somebody, or is a “VIP”, or Dr. so-and-so wants to keep them “one more day”, or there is some bed availability issue. Why in the world you would want to subject your “VIP” to the perils of ICU care any longer than absolutely necessary is beyond me. How would that look if the Governor dies of C.Diff or a CAUTI on the tail end of an unnecessary extension in their ICU stay?
For more detail on making patient focused risk:benefit assessments I have the resident listen to episode 11.
Getting ready for ICU rounds
I discussed my routine for evaluating new ICU patients in preparation for patient care rounds in episode 20.
My 5 step pre-rounding process:
1. Read the history & physical, consult, and progress notes to determine who is the patient and why are they here
2. Review home medications
3. Review labs, cultures and imaging reports
4. Review the bedside flow sheet
5. Review current medications
More details, including how long I spend pre-rounding on each patient and how I decide which patient to see first are in episode 20.
How to participate in ICU rounds
I’ve developed specific timing and methods for how I participate in ICU rounds and present my recommendations. Many recommendations are presented directly on rounds while some are presented outside of rounds using sticky notes.
If a provider hasn’t formally seen & written a note on the patient yet, I make sure to acknowledge that when delivering a recommendation.
Understanding the goals of care for the patient is essential before providing a recommendation on rounds. I like to use a “blind golf caddy” analogy as a frame of reference. A caddy knows the ins and outs of when and how to use each club, just like the pharmacist should know the ins and outs of when and how to use each drug. But we can’t always see the course clearly and need to clarify the goals of care first.
I cover participation in ICU rounds in detail in episode 21.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
Leave a Reply