In this episode I’ll:
1. Review how to recognize severe hyperkalemia
2. Review the 3 categories of hyperkalemia treatments and the order which they should be used
3. Discuss the nuances of each treatment
Recognizing hyperkalemia
Severe hyperkalemia can be recognized by cardiac conduction abnormalities on ECG, muscle weakness / paralysis, or a serum potassium value greater than 7. In a patient without chronically high potassium, a value lower than 7 may still have severe consequences.
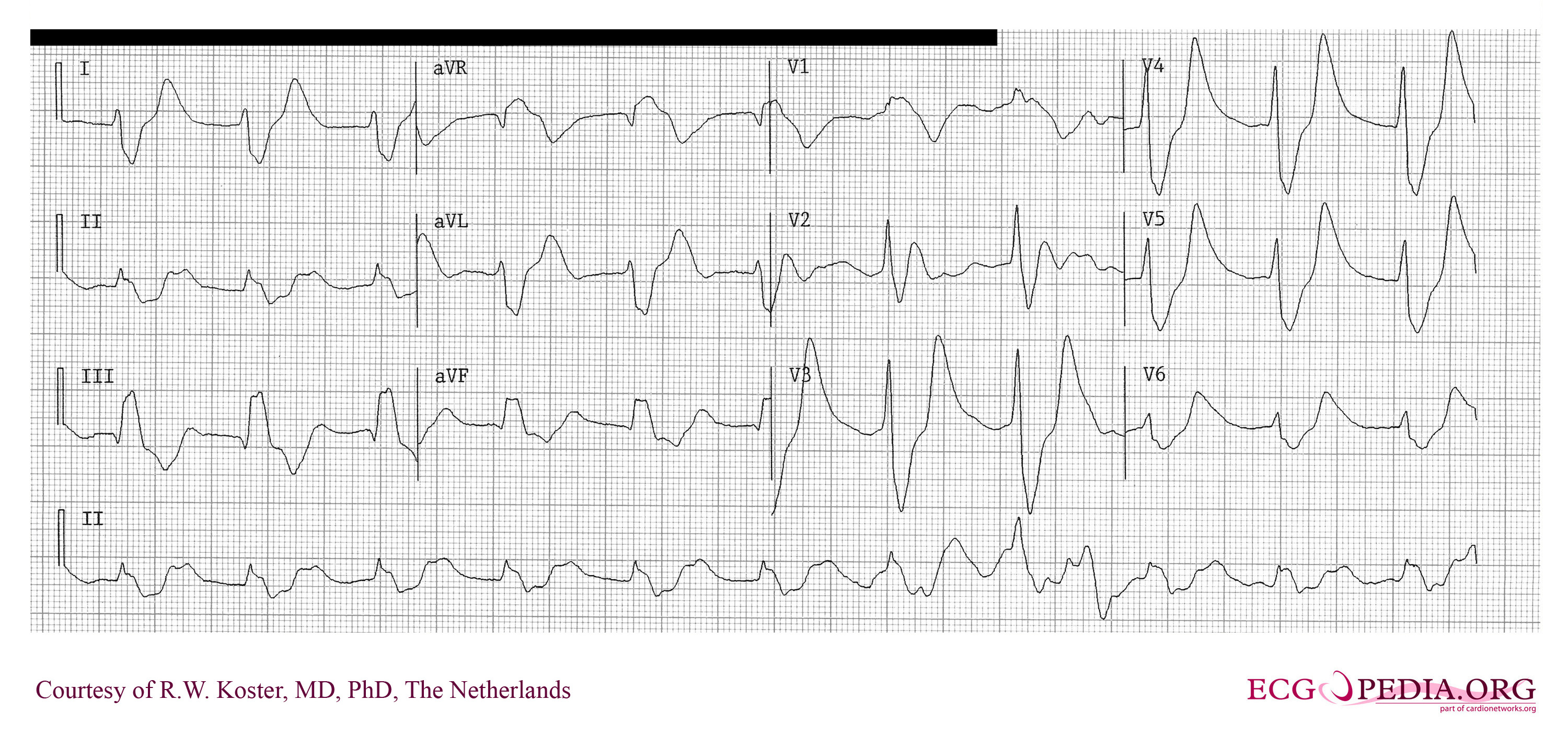
While a patient with severe hyperkalemia can progress from any level of ECG change to ventricular tachycardia / ventricular fibrillation / asystole, in general a peaked T wave with shortened QT interval is the earliest change, followed by progressive lengthening of the PR interval and QRS duration. The P wave may disappear, and ultimately the QRS widens further to a sine wave until asystole occurs. Don’t bother trying to learn at which level of potassium the ECG changes occur – the changes do not correlate well with the serum potassium concentration.
An ECG from a patient with a serum potassium of 7.5 with flattened P waves, widened QRS interval, and peaked T waves:
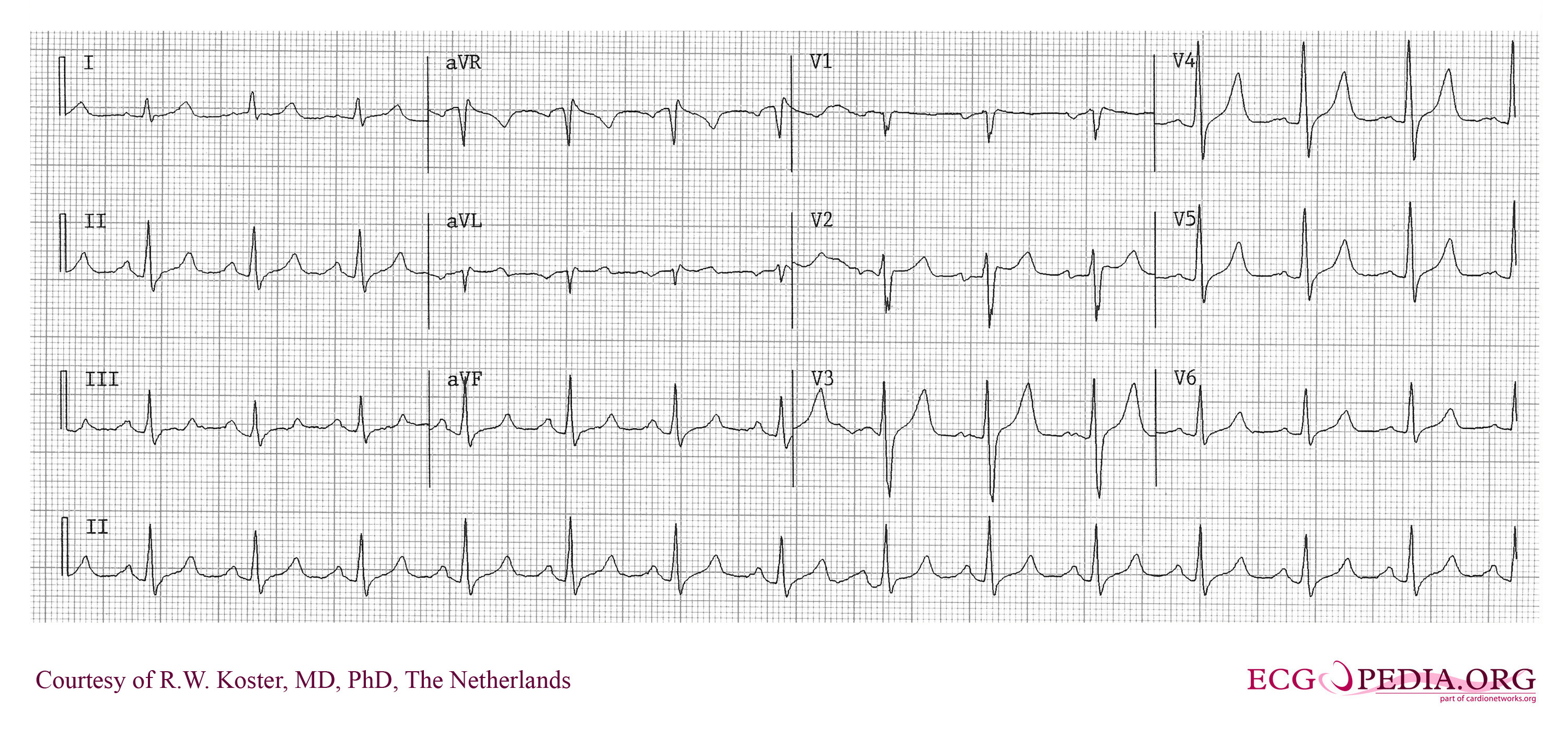
An ECG from the same patient after correction of the serum potassium has begun. Note the T waves remain peaked but the P waves and QRS interval have normalized:
If hyperkalemia is suspected and you don’t have point of care testing, the fastest way to get the serum potassium is to send a venous blood gas (VBG) sample to the lab for analysis. Sending a VBG is the fastest way to get a sodium, potassium, glucose, and free calcium level at my hospital with a turn-around time of 15 minutes or less.
Hyperkalemia treatment
Treatment of severe hyperkalemia should follow a 3 step process. In my experience a pharmacist at the bedside can play a significant role in ensuring the steps are followed in the proper order. The steps are:
1. Protect the cardiac membrane with IV calcium
2. Hide the potassium from the heart
3. Remove the excess potassium from the patient
Protect the cardiac membrane with IV calcium
IV calcium works within minutes to protect cardiac membranes from the deleterious effects of hyperkalemia. Two forms of calcium are available to be given IV, and they have a few important differences. The two forms are calcium chloride and calcium gluconate.
Calcium chloride can be given IV push, but causes a significant amount of phlebitis and tissue injury in extravasation so it is best used if there is a life threatening arrhythmia present or a central line is in place. The dose for severe hyperkalemia is 1 gram IV push over 1 minute.
Calcium gluconate is less potent, and causes less irritation. It must be given at a slower rate of 150 mg/minute to avoid hypotension. Calcium gluconate is best used if the patient has a small, peripheral IV line and can tolerate waiting ~15 minutes for the dose to infuse. The dose for severe hyperkalemia is 2-3 grams IV infusion over 15-20 minutes.
Whether calcium chloride or calcium gluconate is used, the dose should be repeated if the ECG change has not normalized within 5 minutes of administration.
The cardiac membrane stabilization effects of calcium last 30-60 minutes, so immediately following calcium administration it is time to work on moving the excess potassium into the intracellular space where it won’t harm the cardiac membrane.
Hide the potassium from the heart
The intracellular concentrations of sodium and potassium are essentially the reverse of the plasma concentrations. This is why a couple extra mEq/L of potassium doesn’t do any harm inside cells, but has a tremendous impact on the outside of cells.
While there are 3 strategies for moving potassium inside of cells, only one of them is worth considering routinely in patients with hyperkalemia. The strategies are:
1. IV insulin (followed by IV dextrose to prevent hypoglycemia)
2. High dose nebulized albuterol
3. IV sodium bicarbonate
IV insulin
I think of insulin like a key that unlocks a door in cell membranes to allow glucose, potassium, and water to walk through. Giving 10 units of regular insulin IV should be enough to lower the potassium to a safe level. This should be followed with 25-50 grams of IV dextrose to prevent hypoglycemia. Even if the patient is already hyperglycemic, some IV dextrose should be given to ensure hypoglycemia does not develop. Either way, it is prudent to check a fingerstick 1 hour after giving IV insulin+dextrose to treat hyperkalemia.
High dose nebulized albuterol
Nebulized albuterol is effective at moving potassium inside cells, but the necessary dose of 20 mg is not practical to give. 20 mg is 4 to 8 times the usual dose for asthma. You’ll need undiluted albuterol for nebulization to give 20mg, and I can’t imagine how bad the side effects of tachycardia & tremor would be! I’ve never encountered a clinical scenario where I thought this was the thing to do and I can’t think of a scenario I’d use this treatment strategy in.
IV sodium bicarbonate
Sodium bicarbonate administration will not have an effect on potassium levels until several hours of a bicarb infusion have elapsed. After 4-6 hours, if the patient with hyperkalemia also had metabolic acidosis, the serum potassium will decrease by just over 0.5 mEq/L. That is not enough to make a difference for a patient with severe hyperkalemia. I think sodium bicarbonate’s only role would be as an adjunct to insulin+dextrose in a patient with concomitant metabolic acidosis.
Remove the excess potassium from the patient
Now that we have protected the patient’s heart from potassium, and moved the extra potassium inside cells, it is time for definitive removal of the extra potassium from the patient.
The treatment that immediately comes to mind – sodium polystyrene sulfate – may not be effective at all for the treatment of acute, severe hyperkalemia!
Sodium polystyrene sulfate (SPS) is a cation exchange resin, and trades a harmless sodium ion for a potassium ion in the lumen of the GI tract. The best evidence available suggests that this medication is no more effective than laxative use for lowering serum potassium levels. While not common, this medication can cause intestinal necrosis, a potentially fatal complication. Certain conditions lead to a higher incidence of intestinal necrosis from SPS and should be considered absolute contraindications to use:
-Postoperative patients
-Patients with an ileus or who are receiving opioids
-Patients with a bowel obstruction
For severe hyperkalemia the treatment of choice to remove excess potassium is hemodialysis. After hemodialysis, expect the potassium concentration to rebound. For this reason you should wait a bit after hemodialysis completes to remeasure the serum potassium.
If hemodialysis is not readily available, and the patient has one of the contraindications listed above to SPS, the patient should be managed with bolus or continuous infusions of insulin and dextrose until arrangements for dialysis can be made.
I should note that a new potassium exchange resin – patiromer – has been approved in the US. However this resin has not been studied in the treatment of acute hyperkalemia and there are no trials registered on clinicaltrials.gov examining patiromer for this indication.
Some additional resources on the topic of hyperkalemia:
A review article Critical Care Medicine
A podcast from emcrit.org discussing the problems with sodium polystyrene sulfate
Ion-exchange resins for the treatment of hyperkalemia: are they safe and effective?
I want to let you know about the Pharmacy Nation Slack group. This is a free group with other pharmacists from around the world collaborating with each other using real-time messaging to help better care for patients. I hope you join me and the over 90 other Pharmacy Nation members there! You can sign up at pharmacynation.org.
Since I’ve started this podcast, I’ve noticed there are a lot of pharmacists and other medical professionals sharing their expertise with the world using blogs, Facebook pages, and Twitter accounts. But there are only a handful of high quality medical podcasts that are being published regularly. I’m hoping to change that. That’s why I’m putting together a step-by-step course on how to start a medical podcast – so that other medical professionals can bring their knowledge, expertise, and voice to the world of podcasting. To learn more about the course, and to sign up to be notified when it is available, head over to howtostartamedicalpodcast.com.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
Good post. I think a lot of residents tend to overtreat mild hyperkalemia. The other things I’ve noticed are the over use of bicarbonate and SPS and the under use of albuterol (though you point out the relevant issues with feasibility), and the lack of a follow-up fingerstick. What do you think about furosemide as part of the treatment of acute hyperkalemia (excluding anuric patients)?
Thank you! If the hyperkalemia is severe, I’d still prefer hemodialysis since I’m not aware of any evidence that furosemide has a meaningful impact on the serum potassium in an acute setting. But for less-than-severe hyperkalemia in a patient with adequate renal function I think they are a useful treatment.
I believe your before and after EKGs are the same. . .
You are absolutely correct! Thank you so much for catching that – I’ve fixed the second tracing.
Pharmacist Joe, great podcast! I learned something new :).
Thank you for the explanation of the difference between Calcium Gluconate and Calcium Chloride– very important info for a nurse who has to take care of the postop patients and had a few patients developing arrhythmia in the middle of the night.
I didn’t known the contraindications for Kayexalate and its major side effect. Now, I know.
Thank you very much!!
One small request: can you also use a common name for medication you talk about, like Kayexalate. Though, now I know that it is Sodium Polystyrene Sulfate. 😉
A few questions:
1. Can protection of the heart with Ca Gluconate or Calcium Chloride and decrease of the level of potassium with insulin be done simultaneously if the patient has more than one IV site?
2. When we administer insulin SQ for our diabetic patients, does it affect the level of potassium (i did’t notice)? or only IV administration of insulin has this effect?
Thank you again for your website and podcast!
Thank you Inka! I’m glad you like the website & podcast! I’d be honored if you left a review at pharmacyjoe.com/iTunes.
Great suggestion to also use the brand name for medications!
To answer your questions – if you have 2 nurses to administer the calcium simultaneously with the insulin, go ahead and do so. But if it is just one nurse in the room, the priority should be for the calcium.
Insulin to some level is going to force potassium inside cells whether the person has hyperkalemia or a normal potassium level. I’ve never heard of a patient becoming significantly hypokalemic from subcutaneous insulin though.
Thank you.
Thank you for another great post! There is a new potassium binding resin called patiromer approved in October 2015. I haven’t read the trials yet but interested to learn what (if any) advantages it has over SPS.
Thank you MandyO! Unfortunately patiromer has not been studied for acute hyperkalemia. Last time I checked clinicaltrials.gov there was nothing in the works…maybe someday!
Great post! Love the way you explain things.