Most third-party drug interaction services or references don’t help with determining the clinical significance of a given drug interaction. But the book Top 100 Drug Interactions by Hansten and Horn helps me determine whether an interaction is real vs theoretical, so I can guide patients and physicians safely through the complicated arena of drug interactions.
This book is my all-time favorite reference book on drug interactions, and I have purchased it every year for well over a decade.
I especially appreciate how the authors are willing to accurately state the risk of potential drug interactions, and only include in the book interactions they feel are clinically significant. This makes Top 100 Drug Interactions a guide that can be counted on to provide practical advice for managing drug interactions, without any unnecessary fluff.
The book has 10 sections but I find myself using 3 of them over and over again in my practice.
The first of these sections is the cytochrome p450 interaction table.
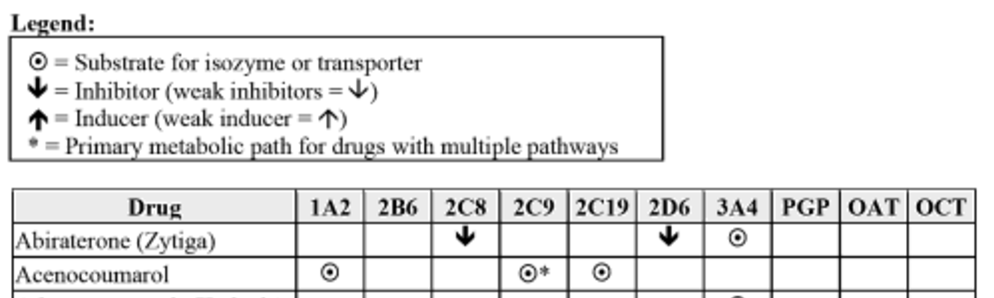
Not all drug interactions are known, and new drugs arrive on the market with limited drug interaction data. To allow clinicians to predict pharmacokinetic drug interactions in unstudied combinations, Hansten and Horn publish an extensive table of medications that affect and are affected by the cytochrome P450 system, as well as other transporters such as p-glycoprotein:
This table allows clinicians to identify interactions between enzyme inhibitors, inducers, and substrates. In addition, if a medication has a primary pathway of elimination, it is identified in the chart. This extra piece of information can be used to hypothesize the degree to which an interaction may be significant. For example, although amitriptyline is metabolized by 1A2, 2C19, 2D6, 3A4, and PGP, the primary pathway of elimination is 2D6. Using this information a clinician may choose to allow the use of a 3A4 inhibitor with amitriptyline with the knowledge that many other pathways for elimination exist.
The second section I frequently use is the top 100 drug interaction monographs.
These monographs provide practical information on how to address specific drug interactions including suggested alternatives for either drug involved in the interaction as well as actionable monitoring strategies.
The classification system for drug interactions used in the book is as follows:
Class 1 – There is no situation where the benefit outweighs the risk (such as pseudoephedrine plus a monoamine oxidase inhibitor).
Class 2 – Avoid use unless there is no alternative or the interaction is desired (such as warfarin plus aspirin).
Class 3 – An increased risk exists but monitoring may be an acceptable course of action (such as low doses of fluconazole with 3A4 substrates).
Class 4 – Minimal risk.
Class 5 – No interaction.
Although the guide contains far more than 100 potential drug interactions, the authors do a superb job focusing on only the clinically relevant interactions that are class 1, 2, or 3.
The third section I frequently use is the one for evaluating QTc interactions.
My method for evaluating QTc interactions draws strongly from Hansten and Horn’s book and I discuss it extensively in episode 12.
I highly suggest if you have not already read episode 12 about QTc drug interactions that you take a moment to do so. In brief, two things I keep in mind about QTc drug interactions are:
1. Be risk-averse whenever possible. Take for example a patient with no allergies on sotalol prescribed levofloxacin for CAP. As long as their renal function is good this is a low-risk interaction that I could just monitor. But ceftriaxone plus doxycycline is just as good for CAP and completely avoids the risk of torsades. Why would I take the risk when I have another 1st line treatment that doesn’t include the torsades risk?
Things get murkier when you are having to decide between using a 2nd line drug or monitoring the interaction. Take the same patient but give them anaphylaxis to penicillin. Would vancomycin plus aztreonam plus doxycycline provide the best cure for their pneumonia? How do I balance the added risk of toxicity that using vancomycin brings? Sticking with the levofloxacin and monitoring the patient in the hospital might be more reasonable here, and this brings me to my 2nd point.
2. ECGs are cheap and non-invasive. You should have no hesitation asking for one if the purpose is to evaluate or monitor a QTc drug interaction. Literally, the cost to the hospital is the ink and paper – the machine and technician salary have been paid for already and this fixed cost doesn’t enter into the equation.
You can order a copy of the Top 100 Drug Interactions on Amazon by clicking here.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.

Leave a Reply