In this episode I’ll share the decision making process I use to decide when and how to write a pharmacy progress note.
When to write a pharmacy progress note?
Not all communication is appropriate for a progress note. There are 3 main ways that I communicate with other members of the medical team. They are:
-Verbal communication (in person or on the phone)
-Sticky notes (or other communication not part of the medical record)
-Progress notes
Verbal communication
If a recommendation can’t wait until the next time the chart is read, or I am responding to a provider’s request for help, I will have an in person or telephone conversation with the provider. In person conversations are always preferred, and I will not hesitate to go wherever the provider is in the hospital if possible.
Sticky notes
I often use sticky notes in the morning before ICU rounds. I am mindful that much of a pharmacist’s job involves advising providers to change what they have already ordered.
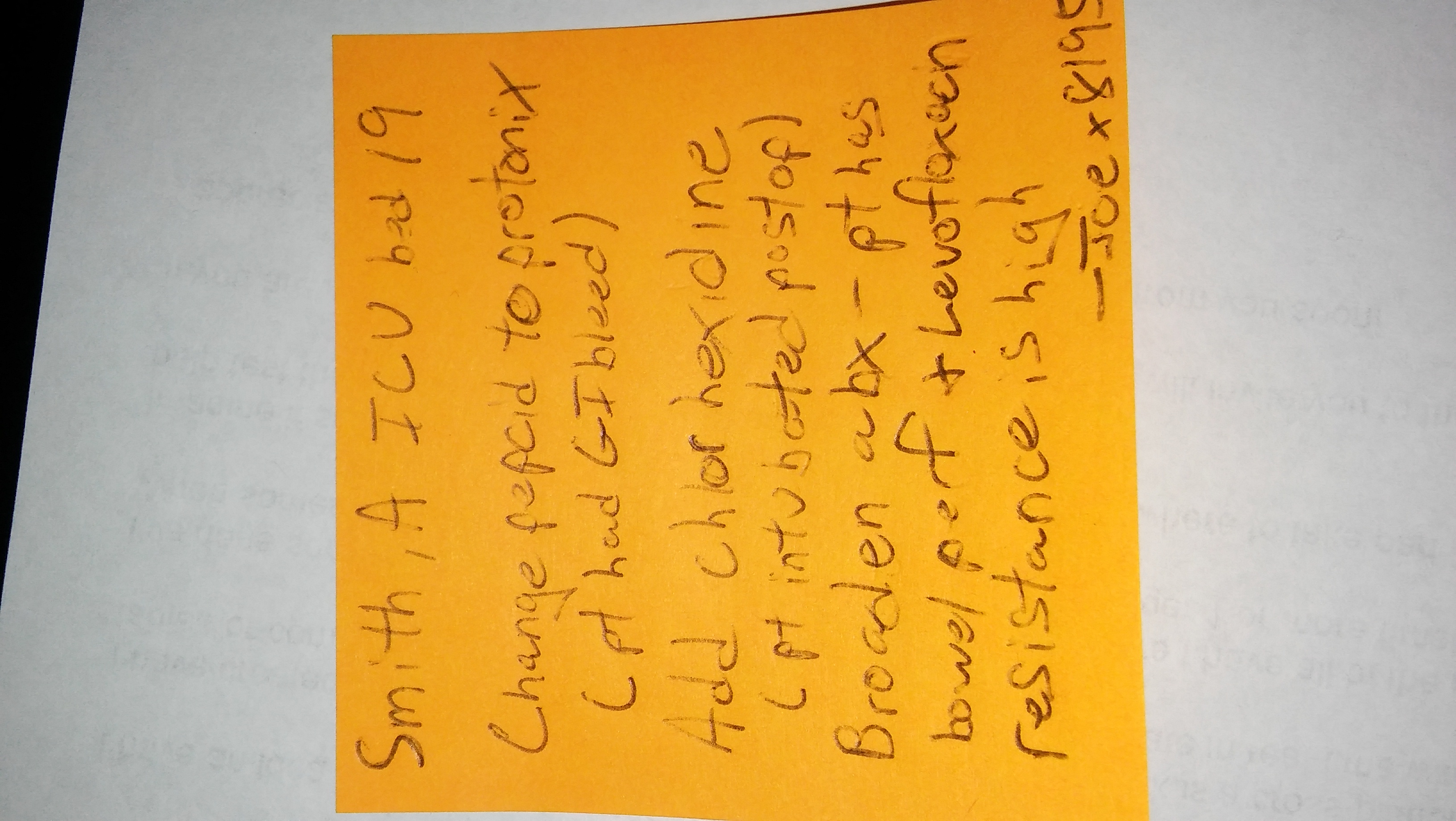
While I’ll never phrase things this way to a provider, on a very basic level I am saying “Don’t do that, do this instead.” To maintain positive relationships with providers I try to minimize the amount of time I am providing recommendations in a public forum like ICU rounds. Sticky notes help with this – here is an example:
A patient originally admitted for GI bleed went to the OR for a perforated bowel. All of their orders were rewritten post-op by the surgical physician assistant. I was seeing the patient in the morning, before the ICU attending. I noted the following issues:
1. The patient had been switched from a PPI to famotidine, but they had a GI bleed earlier in the admission.
2. The patient was intubated but did not have an order for oral care with chlorhexidine.
3. The patient was septic with a perforated bowel but was on levofloxacin (30%+ resistance to e coli) and metronidazole. To find out what I would have recommended in place of levofloxacin check out episode 8 about empiric antibiotic section in the ICU.
I knew ICU rounds would start in an hour or so, but rather than bringing these points up on rounds I left a sticky note on the patient’s flow sheet (which the physician always reviews) similar to this one:
When we rounded later in the morning, I noticed all of my recommendations had been implemented, and I didn’t need to say a thing.
When appropriate, I prefer this sticky note method because it makes the provider look good, and that helps me build my relationship with them.
Progress notes
When it comes to documentation of pharmacy services, I write progress notes in response to a formal consult (pain management, antibiotic monitoring, medication reconciliation, etc…) and whenever there is something I need to communicate to the entire medical team. If there is a grossly ridiculous issue going on, I make sure to call about it rather than write: “Would consider changing synthroid 10 mg po daily to 100 mcg po daily”. It is courteous and helps develop a working-relationship with physicians by not pointing out the above types of errors in a written note that remains part of the permanent record. Also, I will not write a recommendation in the chart that can’t wait 24 hours for implementation (I’ll talk instead).
How to write a pharmacy progress note
There are 3 things I keep in mind when writing a pharmacy progress note:
1. Be brief and to the point
2. Use non-judgmental language
3. Use an alternative to SOAP (subjective, objective, assessment, plan)
Be brief and to the point
No one wants to read a long note with mostly ‘fluff’ in it. Physicians have to read each note. If you write a 3 page note and in the middle suggest a pneumococcal vaccine, the physician doesn’t read it, and the patient goes on to develop pneumonia, you have just left a juicy T-Bone steak for a lawyer to sink their teeth into. Being sued is what goes through a physician’s mind when they are reading a lengthy progress note. If you can say what you need to say in 1 sentence, do it.
Be non-judgmental
When you leave a note, you can’t use body-language or intonation to show that you are genuinely trying to help take better care of a patient with your recommendation. It is easy to be misinterpreted, so I make sure to avoid using judgmental language, such as the word “obviously” or the phrase “should have”. Instead I use non-judgmental words like “consider”.
Use an alternative to SOAP
Physicians write SOAP notes because the SOAP format lends itself well to problem-based care. Pharmacy professors have students write SOAP notes to:
1. See if the student has learned the material.
2. Help the pharmacist understand the physician’s thought process.
In my practice, SOAP notes are usually “overkill” and would result in a lengthy note with lots of ‘fluff’. They would involve lots of copy-pasting of information that did not originate from my expertise (like a physical exam or review of systems).
I remember 10 years ago when I went back to school for my PharmD asking my preceptor, how will I write a note for the “real world”, since it did not seem like the SOAP format would work for my practice. My preceptor didn’t have a specific answer, so I spent a good deal of time on google searching for alternatives to SOAP notes. I finally came across a format that I liked and still use to this day: TITRS. TITRS stands for title, introduction, text, recommendation, signature. I find this format helps me be brief and to the point, yet still communicate the information I feel is necessary in my notes. Here is how I write a pharmacy progress note using TITRS:
The Title & Introduction should answer the basic questions “Who am I? Why am I here? Who is the patient? Why are they here?”
Text should be the subjective & objective information necessary to support your recommendations.
Recommendations should be clear and complete, and followed by your signature and how you can be reached.
Here is a sample note using each of the TITRS components:
Title: Pharmacy – Pain management
Introduction: 58 y/o female post op day 1 s/p small bowel resection and lysis of adhesions
Text: The patient reports 8/10 abdominal pain currently. She is on fentanyl 25mg/hr infusion which has been weaned down from 100mcg/hr since she was extubated this morning. She has COPD, takes morphine IR 30 mg po q6 hrs prn prior to admission, and has used PCA successfully in the past. Her pain is greatest when she moves or is examined/repositioned. Her creatine clearance is ~40 mL/min. She is NPO per surgery. Her comfort goal is 5/10 and she wishes to be able to participate in therapy without the pain limiting her.
Recommendations:
1. Avoid NSAIDs due to low creatinine clearance.
2. D/C fentanyl infusion and start fentanyl PCA as follows: 40 mcg clinician bolus, 10 mcg/hr basal rate, 10 mcg demand dose every 6 minutes, 1 hour lockout of 110mcg.
3. If pain control not satisfactory after 90 minutes on the above settings, increase demand dose and 1 hour lockout by 50% & add continuous pulse oximetry.
4. PCA patient education given.
Signature: Pharmacy Joe
Deciding when to communicate verbally, with a sticky note or in a progress note is a matter of personal judgment. Make sure you are comfortable with whatever method you choose.
Additional resources
You can get an example progress note that uses the TITRS format and a 2-page guide on how to write a progress note in my free download area at pharmacyjoe.com/free. It’s download # 14 on the list.
For more detailed information on writing progress notes, using sticky notes for interventions (sometimes) and documenting clinical services outside of the medical record I have a Masterclass training in the Hospital Pharmacy Academy. Go to pharmacyjoe.com/academy for immediate access.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
very helpful information ..i was really on need of it. i am clinical pharmacist in icu for 3 years but till now not satisfied with my work and feel that i still need training and reading to perform my work properly. i really do benefit from you …thank you very nuch
I’m glad you find it useful! We will always be learning, that is for sure!
Hi. I’ve been practicing as a clinical pharmacist for 7 years and am starting a new position as the critical care pharmacist. Your podcasts are very helpful! I actually had a question about the use of chlorhexidine for prevention of VAP in intubated patients. This is not routine practice at my hospital – I looked up the data and it seems there is evidence it decreases the incidence of VAP, but without any affect on mortality or ICU stay. Just wondering if you have done or have thought of doing a podcast on this topic? Also, any advice on whether I should push to implement this practice in my hospital? Thanks!
Great idea for an episode topic! Check out this Cochrane review on the subject: http://www.cochrane.org/CD008367/ORAL_oral-hygiene-care-critically-ill-patients-prevent-ventilator-associated-pneumonia
Really very good tricks are provided here to write a pharmacy progress notes. This is really very useful for pharmacists, students of PharmD and who are going to start their career in pharmacy.
Thank you!