In this episode, I’ll discuss double anaerobic coverage.
Anaerobic pathogens
Anaerobic pathogens are found in the mouth and the lower gastrointestinal tract. Oral anaerobes are the gram positives Peptococcus and Peptostreptococcus. Intestinal anaerobes are Fusobacterium, Prevotella melaninogenica, and more commonly Bacteroides fragilis.
Oral anaerobes are easily covered with penicillins or clindamycin – think “Anything that a dentist would prescribe.”
Intestinal anaerobes are not as easily covered. Antibiotic coverage against Bacteroides is excellent for metronidazole, piperacillin-tazobactam, and carbapenems. Resistance against these agents is generally less than 1%.
Coverage against Bacteroides is not as good for ampicillin-sulbactam, moxifloxacin, and clindamycin with resistance rates exceeding 35% for the latter 2 of these agents.
Double anaerobic coverage is the combination of 2 or more of the following agents:
Ampicillin/sulbactam
Carbapenems (Doripenem, Ertapenem, Imipenem, Meropenem)
Cefotetan
Cefoxitin
Clindamycin
Metronidazole
Moxifloxacin
Piperacillin/tazobactam
Ticarcillin/clavulanate
Tigecycline
A common antibiotic stewardship intervention is the elimination of double anaerobic coverage. I approach the question of double anaerobic coverage this way:
If an agent with less than 1% chance of resistance vs Bacteroides is already being used, there is no need to add a 2nd anaerobic agent.
If an agent with a high chance of resistance vs Bacteroides is being used, it makes more sense to switch to an agent with low resistance rather than to add a 2nd anaerobic agent.
Examples
For the combination of clindamycin + piperacillin/tazobactam, I would stop the clindamycin since it has a higher resistance rate.
For the combination of metronidazole + a carbapenem, I would stop the metronidazole since the carbapenem covers aerobic pathogens in addition to anaerobic ones.
Guideline confusion
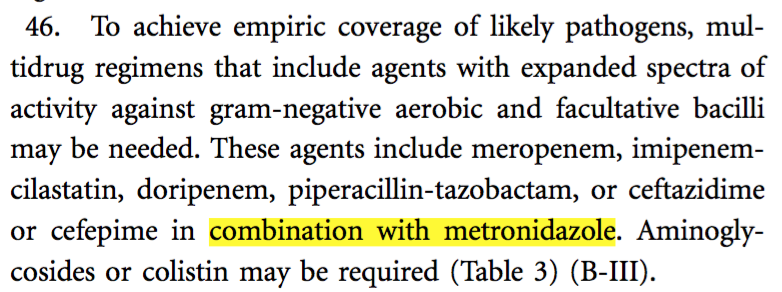
Anyone reading the IDSA guidelines for intra-abdominal infections might be led to believe that double anaerobic coverage is indicated. Take a look at the recommendation:
Reading this recommendation, it is not clear whether the guideline is suggesting metronidazole be added to the other anaerobic agents or only to ceftazidime or cefepime.
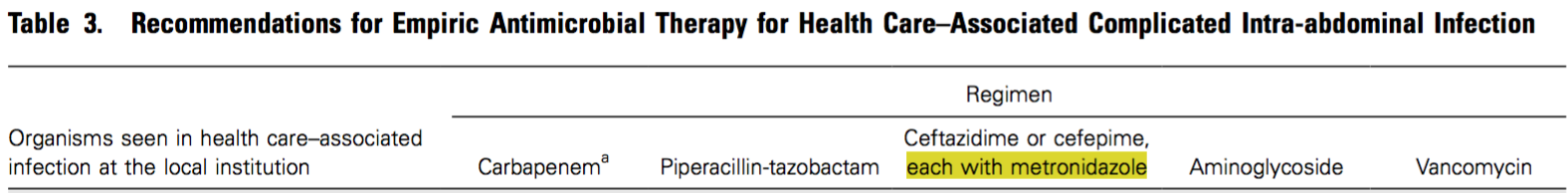
However, in Table 3 of the guidelines it is clear that metronidazole is only to be combined with ceftazidime or cefepime, and not with carbapenems or piperacillin-tazobactam.
Does double anaerobic coverage ever make sense?
There are two scenarios where double anaerobic coverage is appropriate:
1. When a patient has an infection that requires anaerobic coverage AND they require metronidazole for Clostridium difficile infection.
2. When a patient has necrotizing fasciitis and clindamycin is added to reduce bacterial toxin production.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
I actually have a question on whether or not double anaerobic coverage is warranted for deep abscesses, like liver for example and it appears that this https://www.ncbi.nlm.nih.gov/pubmed/1159331 study was cited as one of the literature support on that. Though its only an animal study, when the rat was not double covered, the mortality rate went down with gentamicin, but the rat had abscesses everywhere. What would be your take on this?
Hi Adrienne! I don’t see that as a “double anaerobic coverage” study – am I missing something? Thanks!
Joe
Hello,
In regards to your exceptions to double anaerobic usage:
1. When a patient has an infection that requires anaerobic coverage AND they require metronidazole for Clostridium difficile infection.
Does clostridium difficile infection refer to c.diff diarrhea, or ANY type of c. diff infection (i.e. systemic infection). I had a case recently where a med resident ordered Merrem and Flagyl for a ruptured appendicitis in a patient (I’m an RPh) and she stated Flagyl has better clostridium coverage than merrem. She did finally d/c the Flagyl however. Thanks!
I only consider it a valid combination for c diff infection, not for other bowel infections. I’ve spoken with several ID docs as well who do not see any utility in double anaerobic coverage for fecal peritonitis as long as the agent chosen works well vs bacteroides.
Hello! Just wondering your thoughts on the latter portion of the IDSA guidelines for biliary infections where double anaerobic coverage is recommended (Table 4). I’m unaware of any data that supports this, and in fact the guidelines that IDSA pulls info from for this section do NOT recommend DAC. This is the area where I get the most push back from providers is IAI w/biliary source, since technically, IDSA does actually say DAC is recommended.