In this episode, I’ll discuss stress ulcer prophylaxis in critically ill patients.
Stress ulcers were first described in 1969. Stress ulcers are thought to form due to hypoperfusion to the gastric mucosa associated with critical illness. Various factors including coagulopathy, history of peptic ulcer disease, and prolonged mechanical ventilation are thought to be associated with stress ulcer formation.
In 1999, ASHP published therapeutic guidelines on stress ulcer prophylaxis. These guidelines came with a long list of potential indications for stress ulcer prophylaxis in critically ill patients. Dozens of trials and meta-analyses have examined stress ulcer prophylaxis since the publication of the 1999 guidelines
An update to the guidelines has been anticipated for much of this decade, but publication has been delayed.
According to the Way Back Machine:
In October 2013, stress ulcer prophylaxis guidelines were to be published Q1 of 2014:
By August 2014, the guidelines were said to be due out in Q3 of 2014:
2014 came and went, and the next date given was “Early 2015”:
By the summer of 2015 the guidelines were due out “Late 2015”:
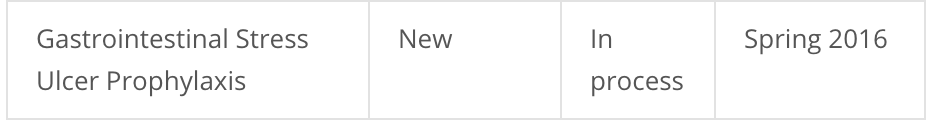
After that deadline was missed, the planned publication date was changed to “Spring 2016”:
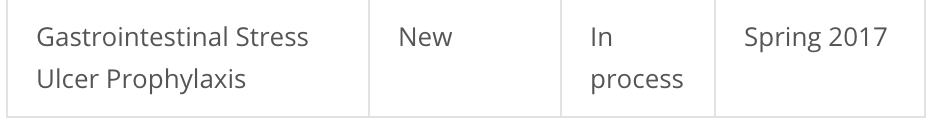
As of this writing, the stress ulcer guidelines are now due out in “Spring 2017”:
If I had to guess the reason for these repeated delays, I would say it is due to conflicting evidence on which ICU patients should be receiving stress ulcer prophylaxis.
In 2013, a systematic review using meta-analysis and trial sequential analysis concluded:
both the quality and the quantity of evidence supporting the use of SUP in adult ICU patients is low. Consequently, large randomised clinical trials are warranted.
Between 2013 and 2014, conflicting data of whether to use histamine-2 antagonists or proton pump inhibitors for stress ulcer prophylaxis were published. One study concluded:
Histamine receptor-2 antagonist therapy appears to reduce costs with survival benefit comparable to proton pump inhibitor therapy for stress ulcer prophylaxis.
Another study concluded:
In critically ill patients, proton pump inhibitors seem to be more effective than histamine 2 receptor antagonists in preventing clinically important and overt upper gastrointestinal bleeding.
In 2015, another meta-analysis was performed, this time in neurocritical patients. Expert opinion of this study was that no firm evidence of benefit or harm exists for stress ulcer prophylaxis in neurocritical patients and that high-quality trials are needed.
Sprinkled throughout recent years are studies which suggest that stress ulcer prophylaxis may be avoided or discontinued in patients who are tolerating enteral nutrition.
Most recently in October 2016 a randomized, placebo-controlled trial of 214 mechanically ventilated critically ill patients suitable for enteral nutrition concluded:
We found no evidence of benefit or harm with the prophylactic administration of pantoprazole to mechanically ventilated critically ill patients anticipated to receive enteral nutrition. The practice of routine administration of acid-suppressive drugs to critically ill patients for stress ulcer prophylaxis warrants further evaluation.
Conflicting and rapidly changing literature findings must make achieving consensus for expert guidelines challenging. In my opinion, whether the evidence is clear as day or clear as mud, the guidelines should be updated. Even a consensus finding that the evidence for prophylaxis is low would give support to clinicians who wish to take rapidly changing evidence into account in their daily practice.
Perhaps the best-case scenario would be for the stress ulcer prophylaxis guidelines to be updated in Spring 2017, and for ASHP to adopt a “living guidelines” model such as what CHEST and ACLS already do. In this way, the guidelines can be rapidly updated as the evidence evolves.
If you like this post, check out my book – A Pharmacist’s Guide to Inpatient Medical Emergencies: How to respond to code blue, rapid response calls, and other medical emergencies.
Thanks for the follow up on this topic, it is really helpful to know where we currently stand.
I want to share the below metanalysis that showed benefit of H2RA over PPI in regards to lower GI hemorrhage, Pneumonia, Cdiff infections, ICU mortality and ICU cost. Based on this metanalysis, our institution mainly use H2RA for ICU patient stress ulcer prophylaxis unless a PPI is indicated.
MacLaren, R et al. Histamine-2 receptor antagonists vs proton pump inhibitors on gastrointestinal tract hemorrhage and infectious complications in the intensive care unit. JAMA Intern Med. 2014 Apr;174(4):564-74. PMID: 24535015
Thanks for the update to no updates! I thought I was the only one waiting for this guideline update. I routinely battle who needs SUP and choice of agent in my daily practice. I am infavor of H2RAs for all unless on PPI prior to admission